What Do You Do When Your Breastfed Infant Has an Allergy or Food Sensitivity?
You suspect your breastfed infant has an allergy or food intolerance and is reacting to proteins in your breast milk, now what? First, consult with your pediatrician and determine if referrals to an allergist or gastroenterologist are warranted. In conjunction with your medical team, the following steps can help guide your journey.
I Think My Breastfed Infant Has an Allergy! Now What?
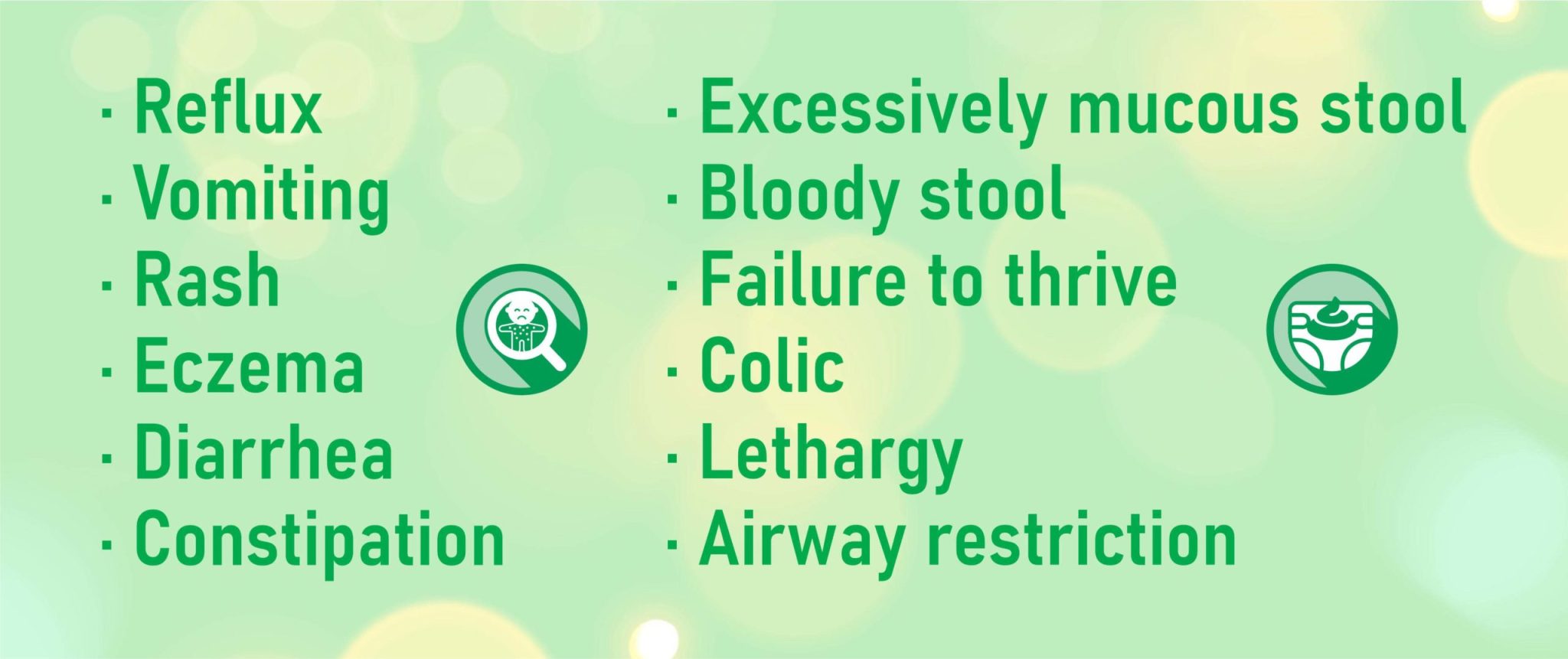
Before jumping into a game plan, lets discuss what warrants it in the first place. The following symptoms can be indicative of an infant food intolerance or allergy: [1]
- Reflux
- Vomiting
- Rash
- Eczema
- Diarrhea
- Constipation
- Excessively mucous stool
- Bloody stool
- Failure to thrive
- Colic
- Lethargy
- Airway restriction
Since these range widely, it is important to consider other contributing factors such as lactation issues, teething, vaccines, or illness before taking action to fix a food problem that may not exist. Additionally, some symptoms which exist solely, such as reflux or colic, may not be attributed to food allergies and options should be discussed with your medical professional. Commonly, two or more symptoms occur when baby is reacting to dietary proteins in your breast milk [1].
Taking Action
This is not a one-size-fits-all issue. The best course of action is different for every mother, infant, and family situation. Here, we outline two courses of action: removing one food at a time or removing all common culprits at once from a mother’s diet. The reason why these two approaches are recommended are based on the pros and cons of each. When removing only one at a time, it is much easier to tell which is the offending food and it can be much easier on mom. Conversely, removing several foods at once can help baby recover faster from symptoms but it will take longer to deduce which items are the problem and such a restrictive diet can be difficult for mom.
Consideration 1: Symptoms
These decisions are often based on symptom severity. Milder symptoms can often be addressed by trialing individual protein elimination until identifying the culprit. Severe symptoms are best addressed by removing most possible culprits and slowly adding back one at a time after symptoms have subsided. For example, a family whose infant has reflux and mucousy stool may want to trial one at a time while a case of severe bloody stool, projectile vomiting, and constant colic may decide to take the second approach and remove several things at once then trial back foods once symptoms are more manageable.
Consideration 2: Dietary Ability
Everyone’s food situation is different. Mothers who plan to remove many food items at once need to consider their nutritional needs and the availability of alternative foods. A helpful outline on less-allergenic food substitutions with similar minerals and vitamins can be found here. Maternal malnutrition is a significant concern if mom cannot access or afford different foods to bridge the nutritional gap.
Consideration 3: Mental Health
There are two opposing maternal mental health considerations. On one hand, continued infant symptoms can be frustrating, depressing, and worrisome. On the other, excessively restrictive diets can be frustrating, depressing, and worrisome. See a theme here? It is vital that moms choose a path which is feasible for their long-term mental health. Breastfeeding is wonderful, but having happy parents is wonderful too. Awareness is key.
How to Remove Individual Foods from Your Diet
When removing an individual food item, understanding timing is vital. What to cut, how long to cut, and if/when to cut the next thing are main questions. Each answer will depend on your situation. We have outlined the top infant food intolerances/allergies below. This is in order of prevalence, so start at the top of the list and choose what to eliminate based on experience. If you are a strict vegan, skip on down to soy as you have already eliminated dairy. If you consume dairy (even lactose free), start there.
The Top 12 Baby Food Allergies are:
- Cow’s Milk Protein
- Soy
- Egg
- Wheat
- Corn
- Legumes
- Peanuts
- Beef
- Oats
- Rice
- Tree nuts
- Chicken
*It is important to know that any food can cause a reaction. This list is the most common allergies based on research [1] but you may find that your child does not fit this list.
Elimination and Symptoms Timing
Research indicates that ingested food proteins peak in breast milk concentration in approximately 2 hours and steadily decrease from there. While there are always outliers, most ingested proteins will clear mother’s system within 24 hours [3-14]. Read more about the supporting data behind non-human proteins in breast milk here.
The next part of the equation is infant symptoms. How long it will take to see improvement varies greatly depending on infant sensitivity, type of reaction, and length and quantity of exposure (a lot of soy over a long period of time versus a little in a short period) [15-17]. Read this article about allergy timing to better understand how this all works. Essentially, complete healing can take several weeks. If you have indeed removed the real allergy food you should see either a plateau (same) or an improvement in symptoms within a week.
CHECK FOR HIDDEN ALLERGEN SOURCES BEFORE YOU REMOVE ANOTHER FOOD!
The biggest misstep in this process is moving on to the next food without properly removing the current target. Imagine, you have eliminated dairy and see steady increase in symptoms instead of improvement. You decide to remove soy, then egg, then wheat…on and on. Several months or weeks go by without improvement when it suddenly dawns on you that your [insert surprise here] contains dairy. Back to square one. That is why it is sooooo important to ensure heavy scrutinization of everything you ingest before removing the next item. Beverages, supplements, medications, and seasonings are common hidden allergen sources [2]. Keeping a detailed food log during this time can help you pinpoint hidden allergens or what your next target should be. Our Free to Feed App available here can help you with this process!
If you are certain you haven’t consumed the elimination target and are seeing significant increases in symptoms after a week it is time to consider the next target. It is recommended to use an additive approach, meaning add the next elimination to your current diet. Infants may be sensitive to more than one item so eliminating one while adding back another can cause more confusion. For example, baby is allergic to dairy and soy. You remove dairy but still experience symptoms several weeks later and decide to cut soy and bring dairy back. Unfortunately, you will continue to see symptoms because both culprits haven’t been removed together. Once you have reached baseline (little to no symptoms) then you can determine if you would like to trial reintroduction.
How To Remove All Allergenic Foods at Once (Elimination Diet)
Removing many or all allergenic food items at once is also known as an elimination diet or total elimination diet (TED). There are two strategies that seem to work well for mothers here. One: remove all “top” infant allergenic foods altogether. Two: removal of everything aside from a few “safes”. Mothers can decide which route to take based on preference. Option one allows for many more food options while option two is much more controlled. Many nursing moms appreciate option two because it takes out a lot of the guesswork and may return baby to symptom-free faster (because there is less room for accidental allergen ingestion).
Total elimination diets are difficult at best and not recommended long-term. Once baby has reached baseline mom should start adding foods back into her diet to prevent malnutrition. Choosing the “safes” can be difficult as well. Generally, ensuring there is a healthy protein, carbohydrate, and fat is absolutely essential. Please work with your medical professional when making these dietary decisions.
Takeaways
Breastfeeding and infant food allergies deserve more than a cookie-cutter response. Every situation is different and should be treated as such. Work with your medical team, keep a food log, and reach out to Free to Feed for additional support through the process. We offer one on one personal consults to help you navigate this space and understand the science behind what is happening for you and your little. You are doing an amazing job, mama!
References
- Luccioli, Stefano, et al. “Maternally reported food allergies and other food-related health problems in infants: characteristics and associated factors.” Pediatrics 122.Supplement 2 (2008): S105-S112.
- Zurzolo, Giovanni A., et al. “Hidden allergens in foods and implications for labelling and clinical care of food allergic patients.” Current allergy and asthma reports 12.4 (2012): 292-296.
- Vadas, Peter, et al. “Detection of peanut allergens in breast milk of lactating women.” Jama 285.13 (2001): 1746-1748.
- Palmer, D. J., M. S. Gold, and M. Makrides. “Effect of maternal egg consumption on breast milk ovalbumin concentration.” Clinical & Experimental Allergy 38.7 (2008): 1186-1191.
- Walker‐Smith, J. A. “Diagnostic criteria for gastrointestinal food allergy in childhood.” Clinical & Experimental Allergy 25 (1995): 20-22.
- Host, Arne, and Susanne Halken. “Cow’s milk allergy: where have we come from and where are we going?.” Endocrine, Metabolic & Immune Disorders-Drug Targets (Formerly Current Drug Targets-Immune, Endocrine & Metabolic Disorders) 14.1 (2014): 2-8.
- Kilshaw, Peter J., and Andrew J. Cant. “The passage of maternal dietary proteins into human breast milk.” International Archives of Allergy and Immunology 75.1 (1984): 8-15.
- Zhu, Jing, et al. “Discovery and quantification of nonhuman proteins in human milk.” Journal of proteome research 18.1 (2018): 225-238.
- Picariello, Gianluca, et al. “Excretion of dietary cow’s milk derived peptides into breast milk.” Frontiers in Nutrition ;6 (2019): 25.
- Troncone, R., et al. “Passage of Gliadin Into Human Breast Milk.” Pediatric Research 20.7 (1986): 696.
- Chirdo, F. G., et al. “Presence of high levels of non-degraded gliadin in breast milk from healthy mothers.” Scandinavian journal of gastroenterology 33.11 (1998): 1186-1192.
- Allen, Katrina J., et al. “Allergen reference doses for precautionary labeling (VITAL 2.0): clinical implications.” Journal of allergy and clinical immunology 133.1 (2014): 156-164.
- Jaime, Beatriz Espín, et al. “Non-IgE-mediated cow’s milk allergy: consensus document of the Spanish society of pediatric gastroenterology, hepatology, and nutrition (SEGHNP), the Spanish association of pediatric primary care (AEPAP), the Spanish society of extra-hospital pediatrics and primary health care (SEPEAP), and the Spanish society of pediatric clinical immunology, allergy, and asthma (SEICAP).” Anales de Pediatría (English Edition) 90.3 (2019): 193-e1.
- Koletzko, S., et al. “Diagnostic approach and management of cow’s-milk protein allergy in infants and children: ESPGHAN GI Committee practical guidelines.” Journal of pediatric gastroenterology and nutrition 55.2 (2012): 221-229.
- Jyonouchi, Harumi. “Non-IgE mediated food allergy.” Inflammation & Allergy-Drug Targets (Formerly Current Drug Targets-Inflammation & Allergy) 7.3 (2008): 173-180.
- Jurewicz, Mary Ann. “Anaphylaxis: when the body overreacts.” Nursing 30.7 (2000): 58.
- Jiang, Wenjun, et al. “A mast-cell-specific receptor mediates Iopamidol induced immediate IgE-independent anaphylactoid reactions.” International immunopharmacology 75 (2019): 105800.
*Check each linked Free to Feed articles for additional references!